The Genitourinary Specialist’s Perspective
An important cause of ectopic pregnancy is pelvic inflammatory disease. Infection leads to damage to the ciliary lining of the fallopian tubes increasing the risk of ectopic pregnancy. A common cause of pelvic inflammatory disease is Chlamydia Trachomatis.
The recognition that the treatment of Chlamydia trachomatis genital infection is a public health priority is a major step forward in trying to reduce morbidity and mortality associated with this sexually transmitted infection. The National Chlamydia Screening Programme (NCSP) is being rolled out across England with clear targets being set to Primary Care Trusts to introduce testing to men and women under the age of 25 years. The introduction of the NCSP and innovative pilot projects, such as the NHS BOOTS pilot programme in London and Cornwall, should significantly increase the numbers of individuals having a test for chlamydia infection. Until the introduction of the NCSP, most chlamydia tests were being taken in genitourinary medicine clinics where over 100,000 cases of Chlamydia trachomatis infection are diagnosed each year. It is important that wherever men or women have a chlamydia test which tests positive, they receive appropriate information about the infection, appropriate treatment and, most importantly, arrange for their sexual partners to be treated to ensure they do not get re-infected when they resume intercourse. There are clear public health benefits by treating contacts of those with a diagnosed infection. Further details on the protocols for the treatment of Chlamydia trachomatis infection can be found under the ‘Guideline’ section on the website of the British Association for Sexual Health and HIV (BASHH): http://www.bashh.org/.
The reason that Chlamydia screening is necessary is because over 80% of women and 50% of men who have Chlamydial genital infection do not have any symptoms at the time of diagnosis. There is evidence that treating infection infection early, before symptoms and signs, will reduce the prevalence of infection and the incidence of pelvic inflammatory disease, ectopic pregnancy, tubal infertility and chronic pelvic pain. It is essential that healthy, sexually active men and women, particularly under the age of 25 years, begin to see having a regular Chlamydia test as part of maintaining their good health, and that this test should prompt them to consider the need for additional testing for other infections such as gonorrhoea, syphilis and HIV.
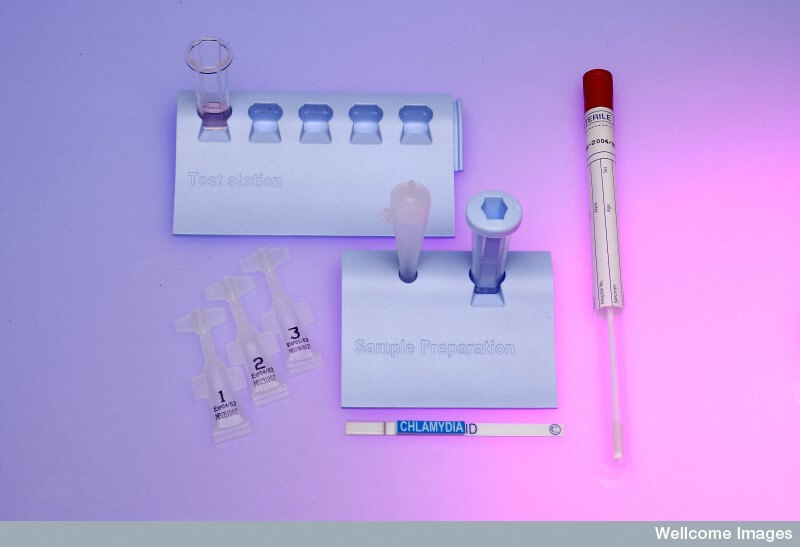
The ease of testing for Chlamydia has been greatly improved by diagnostic technology which means that Chlamydia can be accurately diagnosed by urine testing or, in women, by taking swabs themselves. This means that an important barrier to testing (i.e. the need for a medical examination) is removed for people who are entirely without symptoms.
Automated technology systems now allow the processing of many more samples and the results can therefore be available much more quickly. Furthermore, antibiotic treatment has been reduced to a single dose therapy which is much easier for individuals to take and less likely to result in them having to return because of missed or lost pills. It is important that individuals do recognise, however, that after treatment it is essential to refrain from intercourse until the treatment has worked. A period of one week week is usually recommended, and it is particularly important that they do not resume intercourse with the partner who may have infected them until that partner has also had a test and treatment appropriately.

It is vital in pursuing the goal of reducing the complications of Chlamydia trachomatis infection, particularly its link to tubal damage and ectopic pregnancy, that both men and women receive information about the accessibility of testing for Chlamydia trachomatis infection, and that the National Chlamydia Screening Programme continues to be fully implemented. The benefits to individual women, as well as the significant reduction in NHS tests by reducing complications of Chlamydia trachomatis infection, can only be achieved if sufficient screening programmes are introduced and that individuals are encouraged and enabled to take the test.
Simon E Barton, BSc MD
FRCOG FRCP (Edin) FRCP
Consultant Physician and Clinical Director
HIV/Genitourinary Medicine Services